Knee surgeons play a crucial role in addressing a wide range of knee-related issues, from sports injuries to degenerative conditions. These specialized orthopedic professionals employ various surgical techniques to restore function, alleviate pain, and improve the quality of life for patients with knee problems. Understanding the most common procedures performed by knee surgeons can provide valuable insights into the current state of knee surgery and the options available for those experiencing knee-related issues.
Arthroscopic meniscectomy and meniscus repair techniques
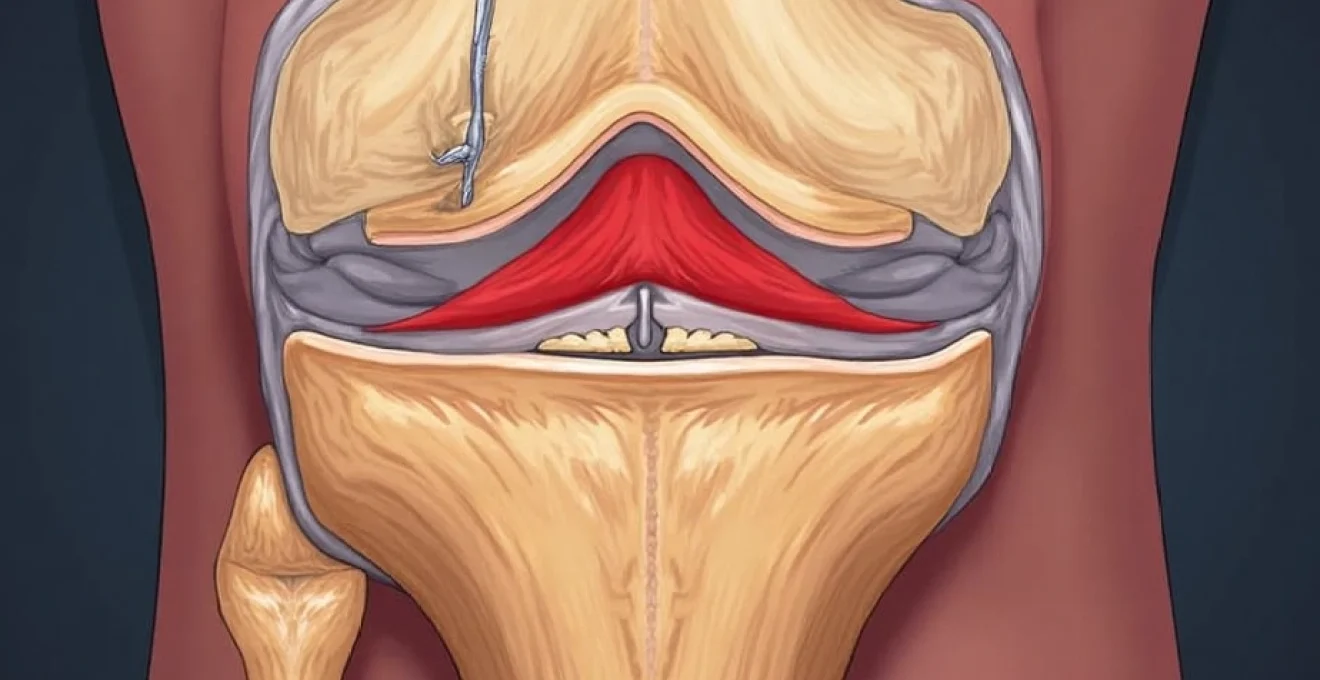
Arthroscopic procedures are among the most frequently performed knee surgeries, with meniscus-related issues being a common reason for intervention. These minimally invasive techniques allow surgeons to diagnose and treat various knee problems through small incisions, resulting in faster recovery times and reduced postoperative complications.
Partial vs. total meniscectomy: indications and outcomes
When dealing with meniscal tears, surgeons must carefully consider whether to perform a partial or total meniscectomy. Partial meniscectomy involves removing only the damaged portion of the meniscus, preserving as much healthy tissue as possible. This approach is generally preferred when the tear is limited to a specific area and the remaining meniscus is structurally sound.
Total meniscectomy, on the other hand, involves removing the entire meniscus. This procedure is typically reserved for cases where the meniscus is severely damaged or degenerative, and repair is not feasible. However, it’s important to note that total meniscectomy can increase the risk of osteoarthritis in the long term.
All-inside meniscus repair: FAST-FIX and NovoStitch plus systems
All-inside meniscus repair techniques have gained popularity due to their ability to address certain types of tears with minimal disruption to surrounding tissues. The FAST-FIX and NovoStitch Plus systems are two innovative approaches that allow surgeons to repair meniscal tears using specialized implants and suturing techniques.
These systems enable precise placement of sutures and anchors, facilitating secure fixation of the torn meniscus. The all-inside approach is particularly useful for addressing tears in the posterior horn of the meniscus, which can be challenging to access using traditional techniques.
Inside-out and Outside-In repair methods: pros and cons
Inside-out and outside-in repair methods are traditional techniques that remain valuable in certain scenarios. The inside-out method involves passing sutures from inside the joint to the outside, while the outside-in approach reverses this direction.
Each method has its advantages and drawbacks. Inside-out repairs offer excellent visualization and precise suture placement but may carry a higher risk of neurovascular complications. Outside-in techniques can be particularly useful for anterior horn tears but may provide less accurate suture placement in some cases.
Meniscal allograft transplantation for severe cases
In cases of severe meniscal deficiency or previous total meniscectomy, meniscal allograft transplantation may be considered. This procedure involves transplanting donor meniscal tissue to replace the missing or severely damaged meniscus. While technically challenging, meniscal allograft transplantation can provide significant pain relief and improved function in carefully selected patients.
Anterior cruciate ligament (ACL) reconstruction
ACL reconstruction is one of the most common knee surgeries performed, especially among athletes and active individuals. This procedure aims to restore stability to the knee joint following an ACL tear, allowing patients to return to their desired level of activity.
Autograft options: patellar tendon vs. hamstring tendon
When choosing a graft for ACL reconstruction, surgeons often consider autografts, which use the patient’s own tissue. The two most common autograft options are the patellar tendon and hamstring tendon.
Patellar tendon grafts are known for their strength and have been the traditional gold standard for ACL reconstruction. They offer excellent initial fixation strength and tend to heal quickly to the bone. However, they may be associated with a higher incidence of anterior knee pain.
Hamstring tendon grafts, typically using the semitendinosus and gracilis tendons, have gained popularity due to their reduced donor site morbidity and potentially lower risk of anterior knee pain. However, they may take longer to fully incorporate and may have a slightly higher risk of graft elongation over time.
Allograft considerations: types and patient selection
Allografts, or donor tissue grafts, are another option for ACL reconstruction. These grafts eliminate donor site morbidity and can reduce surgical time. Common allograft options include:
- Patellar tendon
- Achilles tendon
- Tibialis anterior tendon
- Quadriceps tendon
Allograft selection often depends on surgeon preference, tissue availability, and patient factors. While allografts offer certain advantages, they may have a higher risk of graft failure, particularly in younger, active patients. Careful patient selection is crucial when considering allograft use for ACL reconstruction.
Single-bundle vs. Double-Bundle ACL reconstruction
The debate between single-bundle and double-bundle ACL reconstruction techniques continues in the orthopedic community. Single-bundle reconstruction aims to replicate the anteromedial bundle of the ACL, while double-bundle techniques attempt to recreate both the anteromedial and posterolateral bundles.
Proponents of double-bundle reconstruction argue that it provides better rotational stability and more closely mimics the natural ACL anatomy. However, the procedure is technically more demanding and may not be suitable for all patients. Current evidence suggests that while double-bundle reconstruction may offer some biomechanical advantages, clinical outcomes are often comparable to well-performed single-bundle techniques.
All-inside ACL reconstruction: TightRope RT technique
The all-inside ACL reconstruction technique, exemplified by the TightRope RT system, has gained popularity due to its minimally invasive nature. This approach uses small sockets instead of full tunnels, potentially reducing bone loss and facilitating easier revision surgery if needed.
The TightRope RT technique allows for adjustable graft tensioning and fixation, providing surgeons with greater control over graft placement and tension. While long-term data is still accumulating, early results suggest that all-inside ACL reconstruction can provide outcomes comparable to traditional techniques with the potential for reduced postoperative pain and faster recovery.
Total and partial knee arthroplasty procedures
As the population ages and the incidence of osteoarthritis increases, knee arthroplasty procedures have become increasingly common. These surgeries aim to relieve pain and restore function in patients with severe knee arthritis or other degenerative conditions.
Cemented vs. cementless fixation in total knee replacement
The choice between cemented and cementless fixation in total knee replacement is an ongoing area of research and debate. Cemented fixation has been the gold standard for many years, offering immediate stability and excellent long-term outcomes. However, concerns about cement debris and potential loosening over time have led to increased interest in cementless options.
Cementless fixation relies on biological fixation, with the implant surface designed to promote bone ingrowth. This approach may offer advantages in terms of long-term durability and ease of revision, particularly in younger, more active patients. However, it requires good bone quality and may be associated with a higher risk of early loosening if initial stability is not achieved.
Unicompartmental knee arthroplasty: oxford and zimmer biomet systems
Unicompartmental knee arthroplasty (UKA) is an option for patients with osteoarthritis limited to a single compartment of the knee. This procedure replaces only the affected compartment, preserving more of the patient’s natural anatomy and potentially allowing for a more natural-feeling knee.
The Oxford and Zimmer Biomet systems are two popular options for UKA. The Oxford system features a mobile-bearing design, which may offer advantages in terms of wear reduction and kinematics. The Zimmer Biomet system uses a fixed-bearing design, which some surgeons prefer for its simplicity and reliability.
UKA can provide excellent outcomes in carefully selected patients, with potential benefits including faster recovery, improved range of motion, and a more natural-feeling knee compared to total knee replacement.
Patellofemoral arthroplasty: indications and techniques
Patellofemoral arthroplasty is a specialized procedure designed to address isolated patellofemoral arthritis. This condition affects the articulation between the patella (kneecap) and the femoral trochlea, causing pain and dysfunction during activities that load the anterior knee.
The procedure involves resurfacing the patella and trochlea with specialized implants while preserving the tibiofemoral joint. Proper patient selection is crucial for success, as progression of arthritis in other compartments can lead to poor outcomes. Modern patellofemoral implants have shown promising results in appropriately selected patients, offering significant pain relief and functional improvement.
Robotic-assisted knee replacement: MAKO and ROSA platforms
Robotic-assisted knee replacement has emerged as a cutting-edge technology aimed at improving the precision and consistency of implant positioning. The MAKO and ROSA platforms are two prominent systems in this field, each offering unique features to assist surgeons in preoperative planning and intraoperative execution.
These systems use advanced imaging and real-time tracking to guide bone preparation and implant placement. Potential benefits include:
- Improved implant alignment and sizing
- More precise soft tissue balancing
- Reduced risk of outliers in component positioning
- Potential for improved functional outcomes and implant longevity
While long-term data is still accumulating, early results suggest that robotic-assisted knee replacement may offer advantages in terms of precision and consistency, potentially leading to improved patient outcomes.
Cartilage restoration and repair surgeries
Cartilage injuries can be challenging to treat due to the limited healing capacity of articular cartilage. However, several techniques have been developed to address focal cartilage defects and promote regeneration or repair of damaged cartilage surfaces.
Microfracture and nanofracture techniques
Microfracture and nanofracture are marrow stimulation techniques designed to promote the formation of fibrocartilage in areas of cartilage damage. These procedures involve creating small holes in the subchondral bone to allow bone marrow elements to fill the defect and form a new cartilage-like surface.
Nanofracture is a more recent development that uses smaller, more precise instruments to create the subchondral perforations. This technique aims to minimize trauma to the subchondral bone while potentially improving the quality of the regenerated tissue.
Autologous chondrocyte implantation (ACI) and Matrix-ACI
Autologous chondrocyte implantation (ACI) is a two-stage procedure that involves harvesting the patient’s own cartilage cells, expanding them in a laboratory, and then reimplanting them into the cartilage defect. This technique aims to produce hyaline-like cartilage, which more closely resembles native articular cartilage.
Matrix-ACI is an evolution of this technique that uses a biodegradable scaffold to support the implanted chondrocytes. This approach may offer improved cell distribution and adherence within the defect, potentially leading to better outcomes.
Osteochondral autograft transfer (OATs) procedure
The osteochondral autograft transfer (OATs) procedure involves harvesting small plugs of healthy cartilage and underlying bone from non-weight-bearing areas of the knee and transplanting them into the cartilage defect. This technique provides immediate restoration of the articular surface with hyaline cartilage.
OATs is particularly useful for smaller, focal defects and can provide excellent outcomes in appropriately selected patients. However, it is limited by the amount of available donor tissue and potential donor site morbidity.
Particulated juvenile cartilage allograft transplantation
Particulated juvenile cartilage allograft transplantation is a relatively new technique that uses minced cartilage from juvenile donor tissue. This allograft material is rich in chondrocytes and has shown promise in promoting cartilage regeneration when implanted into cartilage defects.
The procedure is performed in a single stage and may be particularly useful for larger defects where other techniques may be limited. Early clinical results have been encouraging, but long-term data is still being gathered to fully evaluate the efficacy of this approach.
Osteotomy procedures for knee realignment
Osteotomy procedures are designed to realign the knee joint, redistributing weight-bearing forces to relieve pressure on damaged areas and potentially slow the progression of osteoarthritis. These surgeries can be particularly beneficial for younger, active patients who wish to delay or avoid knee replacement.
High tibial osteotomy for medial compartment osteoarthritis
High tibial osteotomy (HTO) is commonly performed to address medial compartment osteoarthritis in patients with varus alignment (bow-legged). The procedure involves cutting the proximal tibia and realigning it to shift the weight-bearing axis laterally, unloading the medial compartment.
Two main techniques for HTO are:
- Opening wedge osteotomy: A wedge is opened on the medial side and filled with bone graft
- Closing wedge osteotomy: A wedge of bone is removed from the lateral side and the osteotomy is closed
The choice between these techniques depends on various factors, including the degree of correction needed and surgeon preference. When performed in appropriate candidates, HTO can provide significant pain relief and functional improvement, potentially delaying the need for knee replacement by several years.
Distal femoral osteotomy for lateral compartment issues
Distal femoral osteotomy (DFO) is less common than HTO but can be an effective option for patients with valgus alignment (knock-kneed) and lateral compartment osteoarthritis. This procedure involves realigning the distal femur to shift the weight-bearing axis medially, unloading the lateral compartment.
DFO can be performed using either opening or closing wedge techniques, similar to HTO. The procedure is technically demanding and requires careful preoperative planning to achieve the desired correction. When successful, DFO can provide significant improvements in pain and function for patients with lateral compartment issues.
Combined osteotomies for complex deformities
In cases of complex knee deformities, combined osteotomies may be necessary to achieve proper alignment. This can involve performing osteotomies at multiple levels, such as combining a HTO with a DFO, or addressing both the coronal and sagittal planes simultaneously.
These complex procedures require meticulous planning and execution but can provide dramatic improvements in knee alignment and function for patients with severe deformities. The use of computer-assisted navigation and 3D printing technology has enhanced surgeons’ ability to plan and execute these challenging cases with greater precision.
Multiligament knee reconstruction and repair
Multiligament knee injuries are complex and challenging cases that require a comprehensive approach to restore stability and function. These injuries often result from high-energy trauma and may involve damage to multiple ligaments, as well as associated injuries to cartilage, menisci, and other soft tissues.
Posterior cruciate ligament (PCL) reconstruction techniques
PCL reconstruction is less common than ACL reconstruction, but it plays a crucial role in restoring knee stability, especially in multiligament injuries. PCL reconstruction techniques have evolved to address the unique biomechanics of this ligament.
The two main approaches for PCL reconstruction are:
- Transtibial technique: Involves drilling a tunnel through the tibia to place the graft
- Tibial inlay technique: The graft is fixed directly to the back of the tibia without a tibial tunnel
Both techniques have their advantages, with the transtibial approach being more common but potentially causing graft elongation over time. The tibial inlay technique may better replicate the native PCL anatomy but is technically more challenging.
Medial collateral ligament (MCL) repair vs. reconstruction
The medial collateral ligament has a good capacity for healing, which often allows for non-operative management or repair rather than reconstruction. However, in cases of severe injury or chronic instability, MCL reconstruction may be necessary.
MCL repair typically involves suturing the ligament back to its insertion point, often augmented with suture anchors. This approach can be effective for acute, isolated MCL injuries with good tissue quality.
MCL reconstruction becomes necessary when the ligament is severely damaged or in chronic cases. Techniques include:
- Anatomic reconstruction using autograft or allograft tissue
- Double-bundle reconstruction to replicate the superficial and deep components of the MCL
The choice between repair and reconstruction depends on factors such as injury severity, tissue quality, and associated injuries.
Posterolateral corner reconstruction: LaPrade technique
The posterolateral corner (PLC) of the knee is a complex structure that plays a crucial role in rotational stability. Injuries to this area often require surgical intervention due to poor healing capacity. The LaPrade technique has emerged as a popular method for anatomic reconstruction of the PLC.
This technique involves reconstructing the three main components of the PLC:
- Fibular collateral ligament (FCL)
- Popliteus tendon
- Popliteofibular ligament
The LaPrade technique uses a combination of grafts to recreate these structures, typically involving both tibial and fibular tunnels. This anatomic approach aims to restore normal knee kinematics and provide long-term stability.
Staged vs. single-stage approaches for multiple ligament injuries
When dealing with multiple ligament injuries, surgeons must decide between a staged approach or a single-stage reconstruction. Each strategy has its advantages and considerations.
Single-stage reconstruction involves addressing all injured ligaments in one operation. Benefits include:
- Shorter overall recovery time
- Potentially earlier return to function
- Reduced risk of arthrofibrosis
However, single-stage procedures can be lengthy and technically demanding, potentially increasing the risk of complications.
Staged reconstruction involves addressing different ligaments in separate surgeries, typically weeks or months apart. This approach may be preferred in cases of severe soft tissue injury or when external fixation is required. Staged reconstruction allows for:
- Focused rehabilitation between stages
- Potentially reduced surgical time and complexity for each procedure
- Opportunity to reassess stability and adjust the surgical plan between stages
The decision between staged and single-stage approaches depends on factors such as injury severity, associated injuries, and surgeon experience. Both strategies can yield excellent outcomes when applied appropriately.